Leaders from the diverse worlds of science and politics have heralded the arrival of a “golden age” of neuroscience. Cutting-edge research is not only enhancing our understanding of the central nervous system, including the brain; it is also driving major advances in medical technology that hold the potential to change the way we diagnose, treat and care for people living with deadly neurological conditions.
One of the most promising developments has been the discovery of a biomarker prevalent among many devastating neurodegenerative diseases – neurofilament. Through the measurement and understanding of neurofilaments, scientists like myself are opening new doors to investigate these diseases, monitor their progression, and develop new therapies. Neurofilaments are proteins that form an essential building block of neurons, which link together to create communications pathways that transmit signals across the brain and spinal cord.1 This complex network of roughly 100 billion neurons enables us to walk, talk and breathe, among hundreds of other essential activities of everyday life.2
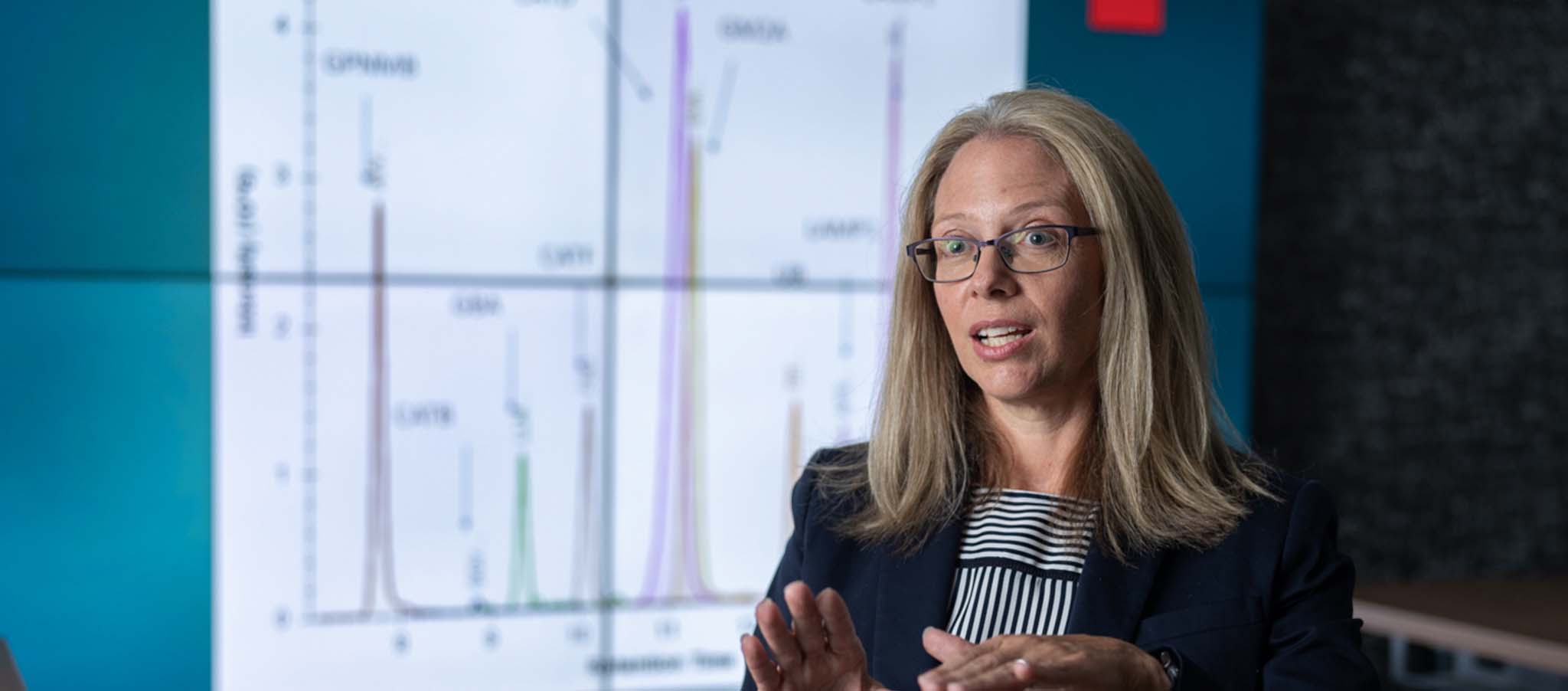
When damage occurs and that network becomes compromised, neurofilaments are released into cerebrospinal fluid (CSF) and the bloodstream. Through numerous academic and industry studies, scientists now recognize that elevated levels of neurofilaments are associated with some of the most devastating neurodegenerative diseases, including amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS), and spinal muscular atrophy (SMA).3, 4, 5
Neurofilaments are released into cerebrospinal fluid (CSF) and blood when neurons are damaged. Scientists are working to create more and more accurate tools (assays) to measure neurofilament in the blood.6